Clinical Study
Are We in a ‘Quademic’? COVID-19, Flu, RSV, and Norovirus Infections Surge
Dr. Pallavi Upadhyay • Feb. 10, 2025
Originally published in: Today’s Clinical Lab
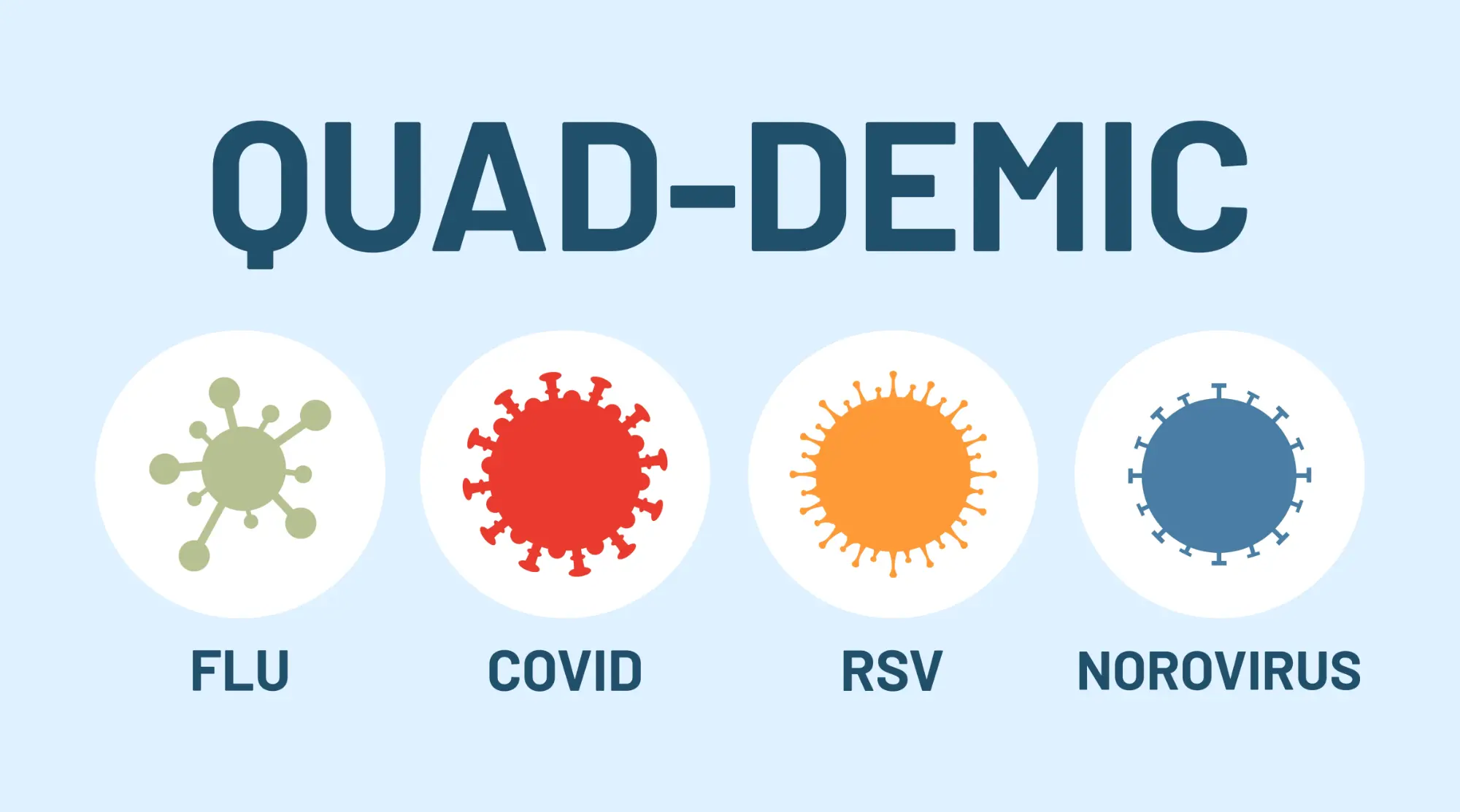
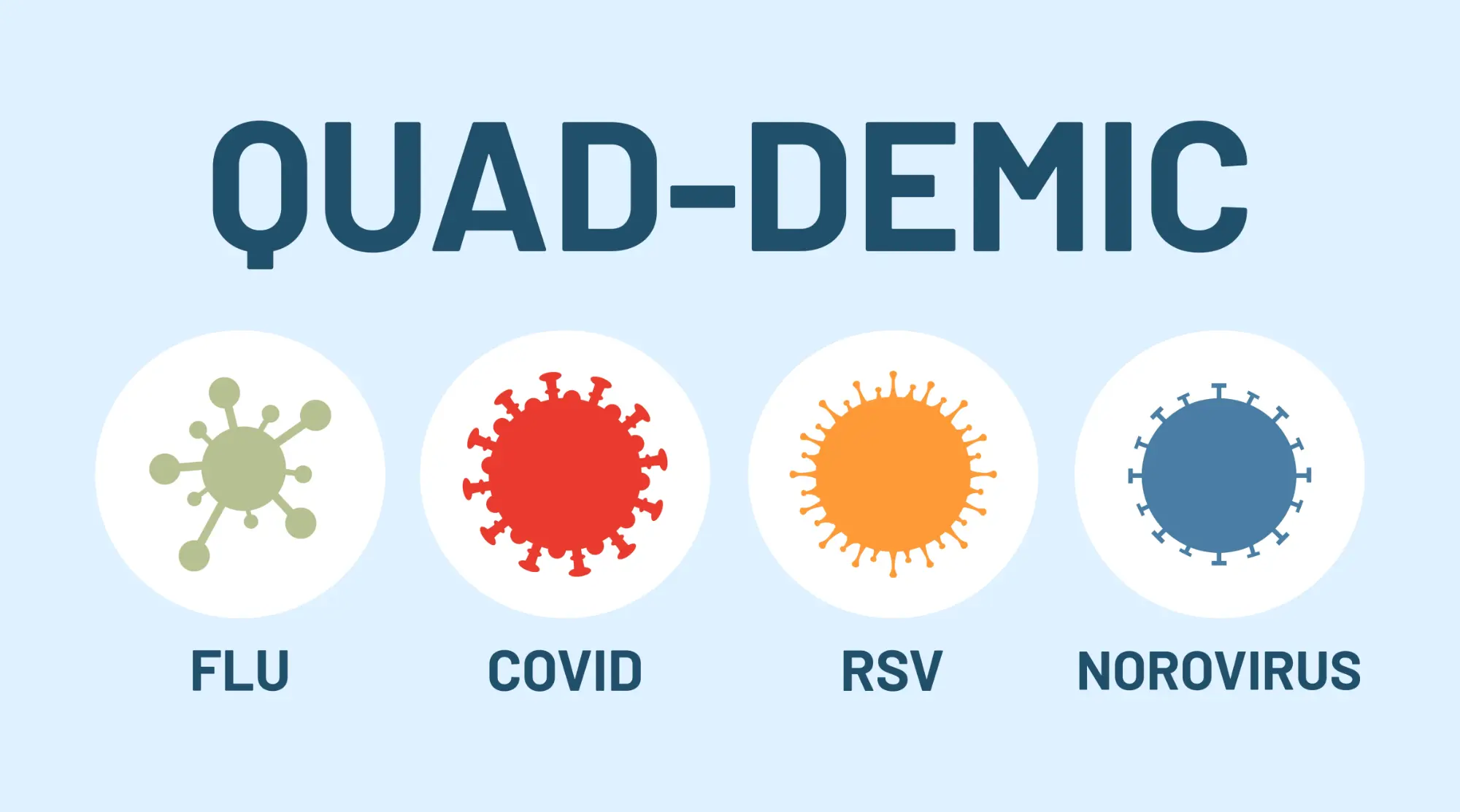
The CDC is also tracking a fourth virus called norovirus after unprecedented outbreaks in 14 states, leading to a “quad demic” this season.
Globally, respiratory tract infections (RTIs) caused by winter viruses pose a significant health and economic threat. Each year in the US, these viruses result in substantial hospitalizations, morbidities, and mortalities, with the healthcare costs (including lost productivity) reaching billions of dollars.1-3 Needless to say, the recent COVID-19 pandemic exacerbated this economic burden significantly.4,5
After all the travel and gatherings of the holidays, the US continues to face a “quademic” this winter, marked by surges in COVID-19, RSV, flu and norovirus infections. Public health experts advise continued surveillance, testing, and treatment measures, including vaccines and non-pharmaceutical interventions, or NPIs, such as social distancing, lockdowns, and international travel restrictions, to prevent the spread of infections.
What is a ‘quad demic’?
By the winter of 2022–2023, SARS-CoV-2, the virus that causes COVID-19, no longer predominated RTIs and influenza like-illness (ILI); instead, the US loomed with a “tripledemic” of influenza viruses, COVID-19, and respiratory syncytial virus (RSV), which substantially overburdened the healthcare system. The winter of 2023–2024 also exhibited a similar respiratory disease season in terms of hospitalizations (albeit higher than pre-pandemic winters).6
This year, the Centers for Disease Control and Prevention (CDC) predicts hospitalization rates will be comparable to the previous season,7 but the agency is also tracking a fourth virus called norovirus—a gastrointestinal virus more prevalent in winter months.
According to CDC reports, an unprecedented outbreak of norovirus is noted in 14 states. The infection spikes are much higher than those reported in the past several years around the same time.8 This quadruple threat (flu, SARS-CoV-2, RSV, and norovirus) in the US is now being unofficially called a “quademic” or “quad-demic” by news outlets.
What is driving the ‘quademic’ in the US?
Some of the main factors driving the quademic include the following:
1. Seasonality of common winter viruses
Common winter viruses start their circulation within the Northern Hemisphere at the beginning of November, peak from December to February, and finally plummet in March/April. These viruses are usually dormant during summer and early fall; however, lower rates of infections can still be seen in asymptomatic as well as symptomatic patient groups mainly comprising of children, the elderly, and people who are immunocompromised.9,10
2. Aftermath of the COVID-19 pandemic
During the ongoing pandemic, strict public health measures enacted in 2020–2021, including non-pharmaceutical interventions such as social distancing, lockdowns, and international travel restrictions, were implemented worldwide to drastically and effectively curb the spread of infection. Epidemiological studies conducted during the pandemic show a significant decline in viral RTIs (VRTIs) caused by viruses other than SARS-CoV-2.11
There are several hypotheses as to why the circulation of non-SARS-CoV-2 winter viruses decreased during the COVID-19 pandemic. The most common explanation was that the NPI measures implemented to combat SARS-CoV-2 were also very effective in reducing common winter VRTIs. Several studies also attributed viral–viral interference, where one virus prohibits the transmission of another, for the reduction in VRTIs during the early peaks of the pandemic.
But what about the current resurgence of VRTIs? Some researchers suggest that the minimal exposure to winter viruses during the pandemic led to an “immunity debt” against these infections,12 which is currently feeding the seasonal and aseasonal epidemics.
3. In-person social interactions
Return-to-work mandates and in-person college settings, as well as an increase in travel and social gatherings this past year, have also contributed to the current surge in VRTIs.
Preparedness against winter flu season
Preparing for the winter respiratory season within the healthcare sector is the key to being able to meet the demands for services.
Preparedness for winter respiratory illnesses may encompass the following broad strategies:
1. Surveillance
Monitoring and tracking infection trends (especially the emergent and re-emergent infections) is crucial to ensure early detection and timely control measures.
Within the US, the CDC and the Council of State and Territorial Epidemiologists (CSTE) are two main agencies involved in surveillance and trend reporting of infectious diseases. These agencies work in establishing various programs and activities with other pertinent agencies (at the national, state, and regional levels) toward infection tracking, disease activity, data collection and interpretation, as well as establishing public health measures against disease outbreaks.
Surveillance enables the healthcare sector to assess disease severity, measure system capacity, and inform decision-making around appropriate diagnostic tests and treatments for patients.
2. Prevention
Infection control measures are paramount in infectious disease prevention, especially during respiratory outbreaks. Both pharmaceutical and non-pharmaceutical interventions are two main strategies in combating the infection transmission.
Non-pharmaceutical interventions
Non-pharmaceutical interventions, or NPIs, are health measures implemented to control the spread of infection, and as the term suggests, these interventions do not involve medications. Some of the personal and community NPIs suggested by the CDC are to stay up-to-date with vaccinations (if available), maintain hygiene, and quarantine or isolate if exposed to a respiratory virus. Environmental NPIs, i.e., the sanitization and sterilization of exposed items, should also be used in both indoor and outdoor settings (especially in the case of airborne respiratory infections) to control and minimize the exposure.13,14
Pharmaceutical interventions
Pharmaceutical interventions, or PPIs, are prevention measures that employ medical interventions. While vaccines are the mainstay of controlling COVID-19, flu, and RSV in pediatric and elderly populations, pre-exposure and post-exposure prophylactic antivirals and antibiotics also play a large role in controlling and containing infections.
For this first time, vaccines for all the three of these RTIs, COVID-19, flu, and RSV, have been available at the same time, giving us an upper hand in combating respiratory illness this season, and beyond. And while there is no vaccine against norovirus yet, vaccine development against norovirus is underway, with potential vaccines currently in clinical trials—Moderna’s mRNA-based norovirus vaccine entered Phase 3 clinical trials in September 2024.15
3. Diagnosis and treatment
The clinical presentation and symptoms of common RTIs are not pathogen-specific and often overlap, making the accurate identification of pathogen(s) responsible for RTIs paramount to receiving timely and targeted treatment. Identifying pathogens is also key to antimicrobial stewardship efforts to reduce unnecessary antibiotic use in cases of viral infections. A timely diagnosis also leads to prompt healthcare intervention to prevent further spread. Diagnostics and treatment really go hand in hand for better patient outcome in VRTIs.
While there are several diagnostic tests available for viral respiratory infections, both the CDC and the Infectious Disease Society of America (IDSA) recommend molecular PCR testing, which is now considered the “standard test” for VRTI detection due to its high specificity and sensitivity.16,17
Remaining challenges
As we navigate this quademic, it is crucial to regularly assess and re-assess the strategies, as well as challenges, associated with the surveillance, diagnosis, and treatment of viral respiratory infections, or VRTIs. Integrated surveillance systems to track common respiratory viruses are being implemented by many countries.18
The last few years of the COVID-19 pandemic have not only brought molecular testing to the forefront of diagnostics but have also underscored the importance of advancing and adapting superior diagnostic tools specifically for pathogen detection. Cost-effective sample collection and rapid molecular testing approaches will continue to play a pivotal role in disease diagnostics and management.
The global pandemic has also spurred the development and innovation of a new generation of vaccines against respiratory pathogens. However, widespread acceptance of these new diagnostic techniques and vaccines remains a challenge, for which we need continued investment in creating robust public health networks and education to overcome.
References
- Molinari NA, Ortega‐Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086‐5096.
- World Health Organization (WHO). WHO Manual for estimating the economic burden of seasonal influenza. Geneva: World Health Organization; 2016:63.
- Putri W, Muscatello DJ, Stockwell MS, Newall AT. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966.
- Forsythe S, Cohen J, Neumann P, et al. The economic and public health imperatives around making potential coronavirus disease–2019 treatments available and affordable. Value Health. 2020;23(11):1427–1431.
- Chen S, Prettner K, Kuhn M, Bloom DE. The economic burden of COVID-19 in the United States: Estimates and projections under an infection-based herd immunity approach. J Econ Ageing. 2021;20:100328.
- CDC. October Update – 2023-2024 Respiratory Disease Season Outlook.
- CDC. 2024-2025 Respiratory Disease Season Outlook – October Update.
- CDC. NoroSTAT Data Table.
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections.Annu Rev Virol. 2020;7(1):83–101.
- Theodoropoulos F, Hüsing A, Dittmer U, et al. Seasonal patterns of common respiratory viral infections in immunocompetent and immunosuppressed patients. Pathogens. 2024;13(8):704.
- Tang JW, Bialasiewicz S, Dwyer DE, et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J Med Virol. 2021;93(7):4099–4101.
- Munro AP, House T. Cycles of susceptibility: Immunity debt explains altered infectious disease dynamics post -pandemic. Clin Infect Dis. 2024; iae493. doi:10.1093/cid/ciae493.
- CDC. Preventing Respiratory Viruses.
- CDC. Prevent Disease Transmission.
- Moderna. Moderna Announces First Participant Dosed in Pivotal Phase 3 Trial of Investigational mRNA Norovirus Vaccine, mRNA-1403.
- Hanson KE, Azar MM, Banerjee R, et al. Molecular testing for acute respiratory tract infections: clinical and diagnostic recommendations from the IDSA’s Diagnostics Committee. Clin Infect Dis. 2020;71(10):2744–2751. doi:10.1093/cid/ciaa508
- CDC. Testing and Respiratory Viruses.
- Eales O, Plank MJ, Cowling BJ, et al. Key challenges for respiratory virus surveillance while transitioning out of acute phase of COVID-19 pandemic. Emerg Infect Dis. 2024;30(2):e230768.
References
- Molinari NA, Ortega‐Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086‐5096.
- World Health Organization (WHO). WHO Manual for estimating the economic burden of seasonal influenza. Geneva: World Health Organization; 2016:63.
- Putri W, Muscatello DJ, Stockwell MS, Newall AT. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966.
- Forsythe S, Cohen J, Neumann P, et al. The economic and public health imperatives around making potential coronavirus disease–2019 treatments available and affordable. Value Health. 2020;23(11):1427–1431.
- Chen S, Prettner K, Kuhn M, Bloom DE. The economic burden of COVID-19 in the United States: Estimates and projections under an infection-based herd immunity approach. J Econ Ageing. 2021;20:100328.
- CDC. October Update – 2023-2024 Respiratory Disease Season Outlook.
- CDC. 2024-2025 Respiratory Disease Season Outlook – October Update.
- CDC. NoroSTAT Data Table.
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections.Annu Rev Virol. 2020;7(1):83–101.
- Theodoropoulos F, Hüsing A, Dittmer U, et al. Seasonal patterns of common respiratory viral infections in immunocompetent and immunosuppressed patients. Pathogens. 2024;13(8):704.
- Tang JW, Bialasiewicz S, Dwyer DE, et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J Med Virol. 2021;93(7):4099–4101.
- Munro AP, House T. Cycles of susceptibility: Immunity debt explains altered infectious disease dynamics post -pandemic. Clin Infect Dis. 2024; iae493. doi:10.1093/cid/ciae493.
- CDC. Preventing Respiratory Viruses.
- CDC. Prevent Disease Transmission.
- Moderna. Moderna Announces First Participant Dosed in Pivotal Phase 3 Trial of Investigational mRNA Norovirus Vaccine, mRNA-1403.
- Hanson KE, Azar MM, Banerjee R, et al. Molecular testing for acute respiratory tract infections: clinical and diagnostic recommendations from the IDSA’s Diagnostics Committee. Clin Infect Dis. 2020;71(10):2744–2751. doi:10.1093/cid/ciaa508
- CDC. Testing and Respiratory Viruses.
- Eales O, Plank MJ, Cowling BJ, et al. Key challenges for respiratory virus surveillance while transitioning out of acute phase of COVID-19 pandemic. Emerg Infect Dis. 2024;30(2):e230768.
Related Articles and White papers
Dr. Pallavi Upadhyay • Feb. 10, 2025
Originally published in: Today’s Clinical Lab
The CDC is also tracking a fourth virus called norovirus after unprecedented outbreaks in 14 states, leading to a “quad demic” this season.
Globally, respiratory tract infections (RTIs) caused by winter viruses pose a significant health and economic threat. Each year in the US, these viruses result in substantial hospitalizations, morbidities, and mortalities, with the healthcare costs (including lost productivity) reaching billions of dollars.1-3 Needless to say, the recent COVID-19 pandemic exacerbated this economic burden significantly.4,5
After all the travel and gatherings of the holidays, the US continues to face a “quademic” this winter, marked by surges in COVID-19, RSV, flu and norovirus infections. Public health experts advise continued surveillance, testing, and treatment measures, including vaccines and non-pharmaceutical interventions, or NPIs, such as social distancing, lockdowns, and international travel restrictions, to prevent the spread of infections.
What is a ‘quad demic’?
By the winter of 2022–2023, SARS-CoV-2, the virus that causes COVID-19, no longer predominated RTIs and influenza like-illness (ILI); instead, the US loomed with a “tripledemic” of influenza viruses, COVID-19, and respiratory syncytial virus (RSV), which substantially overburdened the healthcare system. The winter of 2023–2024 also exhibited a similar respiratory disease season in terms of hospitalizations (albeit higher than pre-pandemic winters).6
This year, the Centers for Disease Control and Prevention (CDC) predicts hospitalization rates will be comparable to the previous season,7 but the agency is also tracking a fourth virus called norovirus—a gastrointestinal virus more prevalent in winter months.
According to CDC reports, an unprecedented outbreak of norovirus is noted in 14 states. The infection spikes are much higher than those reported in the past several years around the same time.8 This quadruple threat (flu, SARS-CoV-2, RSV, and norovirus) in the US is now being unofficially called a “quademic” or “quad-demic” by news outlets.
What is driving the ‘quademic’ in the US?
Some of the main factors driving the quademic include the following:
1. Seasonality of common winter viruses
Common winter viruses start their circulation within the Northern Hemisphere at the beginning of November, peak from December to February, and finally plummet in March/April. These viruses are usually dormant during summer and early fall; however, lower rates of infections can still be seen in asymptomatic as well as symptomatic patient groups mainly comprising of children, the elderly, and people who are immunocompromised.9,10
2. Aftermath of the COVID-19 pandemic
During the ongoing pandemic, strict public health measures enacted in 2020–2021, including non-pharmaceutical interventions such as social distancing, lockdowns, and international travel restrictions, were implemented worldwide to drastically and effectively curb the spread of infection. Epidemiological studies conducted during the pandemic show a significant decline in viral RTIs (VRTIs) caused by viruses other than SARS-CoV-2.11
There are several hypotheses as to why the circulation of non-SARS-CoV-2 winter viruses decreased during the COVID-19 pandemic. The most common explanation was that the NPI measures implemented to combat SARS-CoV-2 were also very effective in reducing common winter VRTIs. Several studies also attributed viral–viral interference, where one virus prohibits the transmission of another, for the reduction in VRTIs during the early peaks of the pandemic.
But what about the current resurgence of VRTIs? Some researchers suggest that the minimal exposure to winter viruses during the pandemic led to an “immunity debt” against these infections,12 which is currently feeding the seasonal and aseasonal epidemics.
3. In-person social interactions
Return-to-work mandates and in-person college settings, as well as an increase in travel and social gatherings this past year, have also contributed to the current surge in VRTIs.
Preparedness against winter flu season
Preparing for the winter respiratory season within the healthcare sector is the key to being able to meet the demands for services.
Preparedness for winter respiratory illnesses may encompass the following broad strategies:
1. Surveillance
Monitoring and tracking infection trends (especially the emergent and re-emergent infections) is crucial to ensure early detection and timely control measures.
Within the US, the CDC and the Council of State and Territorial Epidemiologists (CSTE) are two main agencies involved in surveillance and trend reporting of infectious diseases. These agencies work in establishing various programs and activities with other pertinent agencies (at the national, state, and regional levels) toward infection tracking, disease activity, data collection and interpretation, as well as establishing public health measures against disease outbreaks.
Surveillance enables the healthcare sector to assess disease severity, measure system capacity, and inform decision-making around appropriate diagnostic tests and treatments for patients.
2. Prevention
Infection control measures are paramount in infectious disease prevention, especially during respiratory outbreaks. Both pharmaceutical and non-pharmaceutical interventions are two main strategies in combating the infection transmission.
Non-pharmaceutical interventions
Non-pharmaceutical interventions, or NPIs, are health measures implemented to control the spread of infection, and as the term suggests, these interventions do not involve medications. Some of the personal and community NPIs suggested by the CDC are to stay up-to-date with vaccinations (if available), maintain hygiene, and quarantine or isolate if exposed to a respiratory virus. Environmental NPIs, i.e., the sanitization and sterilization of exposed items, should also be used in both indoor and outdoor settings (especially in the case of airborne respiratory infections) to control and minimize the exposure.13,14
Pharmaceutical interventions
Pharmaceutical interventions, or PPIs, are prevention measures that employ medical interventions. While vaccines are the mainstay of controlling COVID-19, flu, and RSV in pediatric and elderly populations, pre-exposure and post-exposure prophylactic antivirals and antibiotics also play a large role in controlling and containing infections.
For this first time, vaccines for all the three of these RTIs, COVID-19, flu, and RSV, have been available at the same time, giving us an upper hand in combating respiratory illness this season, and beyond. And while there is no vaccine against norovirus yet, vaccine development against norovirus is underway, with potential vaccines currently in clinical trials—Moderna’s mRNA-based norovirus vaccine entered Phase 3 clinical trials in September 2024.15
3. Diagnosis and treatment
The clinical presentation and symptoms of common RTIs are not pathogen-specific and often overlap, making the accurate identification of pathogen(s) responsible for RTIs paramount to receiving timely and targeted treatment. Identifying pathogens is also key to antimicrobial stewardship efforts to reduce unnecessary antibiotic use in cases of viral infections. A timely diagnosis also leads to prompt healthcare intervention to prevent further spread. Diagnostics and treatment really go hand in hand for better patient outcome in VRTIs.
While there are several diagnostic tests available for viral respiratory infections, both the CDC and the Infectious Disease Society of America (IDSA) recommend molecular PCR testing, which is now considered the “standard test” for VRTI detection due to its high specificity and sensitivity.16,17
Remaining challenges
As we navigate this quademic, it is crucial to regularly assess and re-assess the strategies, as well as challenges, associated with the surveillance, diagnosis, and treatment of viral respiratory infections, or VRTIs. Integrated surveillance systems to track common respiratory viruses are being implemented by many countries.18
The last few years of the COVID-19 pandemic have not only brought molecular testing to the forefront of diagnostics but have also underscored the importance of advancing and adapting superior diagnostic tools specifically for pathogen detection. Cost-effective sample collection and rapid molecular testing approaches will continue to play a pivotal role in disease diagnostics and management.
The global pandemic has also spurred the development and innovation of a new generation of vaccines against respiratory pathogens. However, widespread acceptance of these new diagnostic techniques and vaccines remains a challenge, for which we need continued investment in creating robust public health networks and education to overcome.
References
- Molinari NA, Ortega‐Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086‐5096.
- World Health Organization (WHO). WHO Manual for estimating the economic burden of seasonal influenza. Geneva: World Health Organization; 2016:63.
- Putri W, Muscatello DJ, Stockwell MS, Newall AT. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966.
- Forsythe S, Cohen J, Neumann P, et al. The economic and public health imperatives around making potential coronavirus disease–2019 treatments available and affordable. Value Health. 2020;23(11):1427–1431.
- Chen S, Prettner K, Kuhn M, Bloom DE. The economic burden of COVID-19 in the United States: Estimates and projections under an infection-based herd immunity approach. J Econ Ageing. 2021;20:100328.
- CDC. October Update – 2023-2024 Respiratory Disease Season Outlook.
- CDC. 2024-2025 Respiratory Disease Season Outlook – October Update.
- CDC. NoroSTAT Data Table.
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections.Annu Rev Virol. 2020;7(1):83–101.
- Theodoropoulos F, Hüsing A, Dittmer U, et al. Seasonal patterns of common respiratory viral infections in immunocompetent and immunosuppressed patients. Pathogens. 2024;13(8):704.
- Tang JW, Bialasiewicz S, Dwyer DE, et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J Med Virol. 2021;93(7):4099–4101.
- Munro AP, House T. Cycles of susceptibility: Immunity debt explains altered infectious disease dynamics post -pandemic. Clin Infect Dis. 2024; iae493. doi:10.1093/cid/ciae493.
- CDC. Preventing Respiratory Viruses.
- CDC. Prevent Disease Transmission.
- Moderna. Moderna Announces First Participant Dosed in Pivotal Phase 3 Trial of Investigational mRNA Norovirus Vaccine, mRNA-1403.
- Hanson KE, Azar MM, Banerjee R, et al. Molecular testing for acute respiratory tract infections: clinical and diagnostic recommendations from the IDSA’s Diagnostics Committee. Clin Infect Dis. 2020;71(10):2744–2751. doi:10.1093/cid/ciaa508
- CDC. Testing and Respiratory Viruses.
- Eales O, Plank MJ, Cowling BJ, et al. Key challenges for respiratory virus surveillance while transitioning out of acute phase of COVID-19 pandemic. Emerg Infect Dis. 2024;30(2):e230768.
References
- Molinari NA, Ortega‐Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086‐5096.
- World Health Organization (WHO). WHO Manual for estimating the economic burden of seasonal influenza. Geneva: World Health Organization; 2016:63.
- Putri W, Muscatello DJ, Stockwell MS, Newall AT. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966.
- Forsythe S, Cohen J, Neumann P, et al. The economic and public health imperatives around making potential coronavirus disease–2019 treatments available and affordable. Value Health. 2020;23(11):1427–1431.
- Chen S, Prettner K, Kuhn M, Bloom DE. The economic burden of COVID-19 in the United States: Estimates and projections under an infection-based herd immunity approach. J Econ Ageing. 2021;20:100328.
- CDC. October Update – 2023-2024 Respiratory Disease Season Outlook.
- CDC. 2024-2025 Respiratory Disease Season Outlook – October Update.
- CDC. NoroSTAT Data Table.
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections.Annu Rev Virol. 2020;7(1):83–101.
- Theodoropoulos F, Hüsing A, Dittmer U, et al. Seasonal patterns of common respiratory viral infections in immunocompetent and immunosuppressed patients. Pathogens. 2024;13(8):704.
- Tang JW, Bialasiewicz S, Dwyer DE, et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J Med Virol. 2021;93(7):4099–4101.
- Munro AP, House T. Cycles of susceptibility: Immunity debt explains altered infectious disease dynamics post -pandemic. Clin Infect Dis. 2024; iae493. doi:10.1093/cid/ciae493.
- CDC. Preventing Respiratory Viruses.
- CDC. Prevent Disease Transmission.
- Moderna. Moderna Announces First Participant Dosed in Pivotal Phase 3 Trial of Investigational mRNA Norovirus Vaccine, mRNA-1403.
- Hanson KE, Azar MM, Banerjee R, et al. Molecular testing for acute respiratory tract infections: clinical and diagnostic recommendations from the IDSA’s Diagnostics Committee. Clin Infect Dis. 2020;71(10):2744–2751. doi:10.1093/cid/ciaa508
- CDC. Testing and Respiratory Viruses.
- Eales O, Plank MJ, Cowling BJ, et al. Key challenges for respiratory virus surveillance while transitioning out of acute phase of COVID-19 pandemic. Emerg Infect Dis. 2024;30(2):e230768.