Clinical Study
Measles: Is the Recent Outbreak Evidence of Waning Herd-Immunity?
Dr. Azia Evans • Mar. 17, 2025
Measles Virus: Understanding the Basics
Measles is caused by the measles virus, a single-stranded RNA virus belonging to the same virus family that includes mumps, rubella, and parainfluenza virus.
Measles, like these other viruses, is an airborne pathogen transmitted through respiratory droplets, and is known to be one of the most contagious viruses in the world.1 The reproduction number, or R₀ of measles, is estimated to be 12-18.2 This means that a single person with measles can infect 12-18 other susceptible individuals.3 For context, the R₀ of Influenza is between 1-2, while COVID-19 is estimated to be 5-7.4,5
Although the severity of disease from a measle infection can often be mild, only causing complications in 20% of cases. The high rate of transmission means a single positive patient can initiate a significant outbreak.6 Due to the severity of transmissibility, the introduction of the childhood measles vaccine in 1963 had a significant impact on disease transmission, rendering the population no longer susceptible, and essentially halting any further outbreaks from occurring.7
In the present day, as more and more children continue to not receive all their childhood vaccines, the number of people susceptible to a measles infection continues to rise. Allowing more opportunities for the virus to spread and increasing the potential for outbreaks to occur.
Disease presentation
Following initial exposure, the first symptoms of measles typically begin within 11-12 days and include fever, malaise, cough, rhinorrhea, and in some cases conjunctivitis. The hallmark maculopapular measles rash typically occurs 14 days after initial exposure, or 2-4 days after respiratory symptom onset.6 The transmission window, when measles is most often spread, occurs as early as 4 days before the rash begins, and up to 4 days after the onset of the rash.1
Common complications associated with measles infection include ear infections and diarrhea, both occurring in approximately 10% of cases. Less common complications include pneumonia and encephalitis, which can occur in 5% and 0.1% of cases, respectively.8
Vaccination Rates
In the 1980s, measles vaccination rates ranged between 94-98% in the United States. However, in 1990, vaccination rates began to drop to 90% and below. Despite seeing a slight increase in vaccinations in the early 1990s, measles vaccination rates have consistently hovered between 90-92% for the last 10 years.9
Why does this small dip in vaccination rates matter for effectively controlling measles outbreaks? Since measles is such a highly transmissible virus, the more unvaccinated individuals there are in the population, the larger the opportunity for measles to continue to spread when a single infection event occurs. When vaccination rates are high, herd immunity takes effect and limits the potential for spread in the community.
What is Herd Immunity and Why It Matters?
Herd immunity refers to the protection provided to unvaccinated individuals when enough of the population is vaccinated.10 In a sufficiently vaccinated society, those few individuals that are unvaccinated, often due to age or immune status that prevents them from receiving a vaccine, remain protected because the people around them are vaccinated. This prevents the spread of vaccine curable diseases to susceptible unvaccinated individuals, because there aren’t enough susceptible people in the population for the infection to spread efficiently. This is explained graphically in the Community Protection diagram below.11
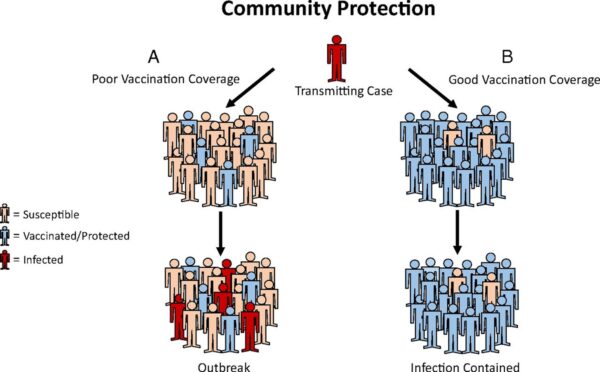
Image sourced from: W.A. Orenstein,& R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).
Herd immunity for measles is considered more critical than for influenza or even COVID-19 because of how highly transmissible the virus is. To achieve effective societal protection, there is a vaccination threshold required. This threshold varies by pathogen and is heavily influenced by the transmission potential (R₀ described above). For measles, specifically, it is estimated that 95% vaccine coverage is required to achieve effective herd immunity. Unfortunately, the United States hasn’t hit 95% vaccination coverage since 1988.9
Conclusions
Taken together, the current outbreak concentrated in Texas, as well as the increasing frequency and severity of measles outbreaks observed over the last several years, provides evidence that the protective herd immunity initially established by the introduction of the measles vaccine is beginning to wane. While there is a sliver of hope that the occurrence of these outbreaks will help to establish immunity in the impacted patients and communities. We will continue to see more incidences like these until 95% coverage is achieved.
References
- Measles. World Health Organization. November 14, 2024. Link
- Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017 Dec;17(12):e420-e428. doi: 10.1016/S1473-3099(17)30307-9. Epub 2017 Jul 27. PMID: 28757186.
- Ridenhour, B., et al. (2018 Dec). “Unraveling R0: Considerations for Public Health Applications.” American Journal of Public Health 108(Suppl 6).
- R, T., et al. (2022 Sep). “Global variation in early epidemic growth rates and reproduction number of seasonal influenza.” International journal of infectious diseases: IJID122.
- Leung, N. H. L. (2021 Mar 22). “Transmissibility and transmission of respiratory viruses.” Nature Reviews. Microbiology 19(8).
- Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 7 Measles. CDC. May 13, 2019. Link
- Measles Vaccination: Know the Facts. Infectious Disease Society of America. November 25, 2024. Link
- Measles Symptoms and Complications. CDC. May 9, 2024. Link
- Measles vaccination coverage. World Health Organization. Link
- Desai AN, Majumder MS. What Is Herd Immunity? JAMA. 2020;324(20):2113. doi: 10.1001/jama.2020.20895
- W.A. Orenstein, & R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).
References
- Measles. World Health Organization. November 14, 2024. Link
- Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017 Dec;17(12):e420-e428. doi: 10.1016/S1473-3099(17)30307-9. Epub 2017 Jul 27. PMID: 28757186.
- Ridenhour, B., et al. (2018 Dec). “Unraveling R0: Considerations for Public Health Applications.” American Journal of Public Health 108(Suppl 6).
- R, T., et al. (2022 Sep). “Global variation in early epidemic growth rates and reproduction number of seasonal influenza.” International journal of infectious diseases: IJID122.
- Leung, N. H. L. (2021 Mar 22). “Transmissibility and transmission of respiratory viruses.” Nature Reviews. Microbiology 19(8).
- Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 7 Measles. CDC. May 13, 2019. Link
- Measles Vaccination: Know the Facts. Infectious Disease Society of America. November 25, 2024. Link
- Measles Symptoms and Complications. CDC. May 9, 2024. Link
- Measles vaccination coverage. World Health Organization. Link
- Desai AN, Majumder MS. What Is Herd Immunity? JAMA. 2020;324(20):2113. doi: 10.1001/jama.2020.20895
- W.A. Orenstein, & R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).
Related Articles and White papers
Dr. Azia Evans • Mar. 17, 2025
Measles Virus: Understanding the Basics
Measles is caused by the measles virus, a single-stranded RNA virus belonging to the same virus family that includes mumps, rubella, and parainfluenza virus.
Measles, like these other viruses, is an airborne pathogen transmitted through respiratory droplets, and is known to be one of the most contagious viruses in the world.1 The reproduction number, or R₀ of measles, is estimated to be 12-18.2 This means that a single person with measles can infect 12-18 other susceptible individuals.3 For context, the R₀ of Influenza is between 1-2, while COVID-19 is estimated to be 5-7.4,5
Although the severity of disease from a measle infection can often be mild, only causing complications in 20% of cases. The high rate of transmission means a single positive patient can initiate a significant outbreak.6 Due to the severity of transmissibility, the introduction of the childhood measles vaccine in 1963 had a significant impact on disease transmission, rendering the population no longer susceptible, and essentially halting any further outbreaks from occurring.7
In the present day, as more and more children continue to not receive all their childhood vaccines, the number of people susceptible to a measles infection continues to rise. Allowing more opportunities for the virus to spread and increasing the potential for outbreaks to occur.
Disease presentation
Following initial exposure, the first symptoms of measles typically begin within 11-12 days and include fever, malaise, cough, rhinorrhea, and in some cases conjunctivitis. The hallmark maculopapular measles rash typically occurs 14 days after initial exposure, or 2-4 days after respiratory symptom onset.6 The transmission window, when measles is most often spread, occurs as early as 4 days before the rash begins, and up to 4 days after the onset of the rash.1
Common complications associated with measles infection include ear infections and diarrhea, both occurring in approximately 10% of cases. Less common complications include pneumonia and encephalitis, which can occur in 5% and 0.1% of cases, respectively.8
Vaccination Rates
In the 1980s, measles vaccination rates ranged between 94-98% in the United States. However, in 1990, vaccination rates began to drop to 90% and below. Despite seeing a slight increase in vaccinations in the early 1990s, measles vaccination rates have consistently hovered between 90-92% for the last 10 years.9
Why does this small dip in vaccination rates matter for effectively controlling measles outbreaks? Since measles is such a highly transmissible virus, the more unvaccinated individuals there are in the population, the larger the opportunity for measles to continue to spread when a single infection event occurs. When vaccination rates are high, herd immunity takes effect and limits the potential for spread in the community.
What is Herd Immunity and Why It Matters?
Herd immunity refers to the protection provided to unvaccinated individuals when enough of the population is vaccinated.10 In a sufficiently vaccinated society, those few individuals that are unvaccinated, often due to age or immune status that prevents them from receiving a vaccine, remain protected because the people around them are vaccinated. This prevents the spread of vaccine curable diseases to susceptible unvaccinated individuals, because there aren’t enough susceptible people in the population for the infection to spread efficiently. This is explained graphically in the Community Protection diagram below.11
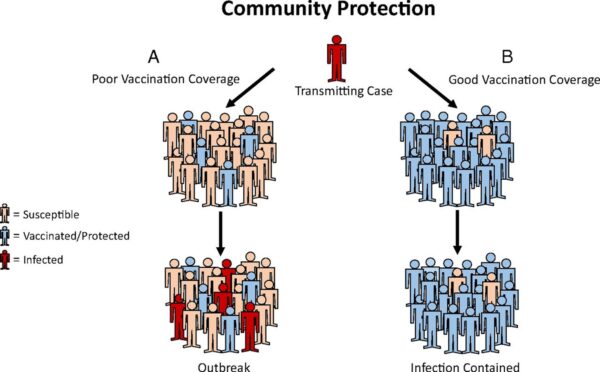
Image sourced from: W.A. Orenstein,& R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).
Herd immunity for measles is considered more critical than for influenza or even COVID-19 because of how highly transmissible the virus is. To achieve effective societal protection, there is a vaccination threshold required. This threshold varies by pathogen and is heavily influenced by the transmission potential (R₀ described above). For measles, specifically, it is estimated that 95% vaccine coverage is required to achieve effective herd immunity. Unfortunately, the United States hasn’t hit 95% vaccination coverage since 1988.9
Conclusions
Taken together, the current outbreak concentrated in Texas, as well as the increasing frequency and severity of measles outbreaks observed over the last several years, provides evidence that the protective herd immunity initially established by the introduction of the measles vaccine is beginning to wane. While there is a sliver of hope that the occurrence of these outbreaks will help to establish immunity in the impacted patients and communities. We will continue to see more incidences like these until 95% coverage is achieved.
References
- Measles. World Health Organization. November 14, 2024. Link
- Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017 Dec;17(12):e420-e428. doi: 10.1016/S1473-3099(17)30307-9. Epub 2017 Jul 27. PMID: 28757186.
- Ridenhour, B., et al. (2018 Dec). “Unraveling R0: Considerations for Public Health Applications.” American Journal of Public Health 108(Suppl 6).
- R, T., et al. (2022 Sep). “Global variation in early epidemic growth rates and reproduction number of seasonal influenza.” International journal of infectious diseases: IJID122.
- Leung, N. H. L. (2021 Mar 22). “Transmissibility and transmission of respiratory viruses.” Nature Reviews. Microbiology 19(8).
- Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 7 Measles. CDC. May 13, 2019. Link
- Measles Vaccination: Know the Facts. Infectious Disease Society of America. November 25, 2024. Link
- Measles Symptoms and Complications. CDC. May 9, 2024. Link
- Measles vaccination coverage. World Health Organization. Link
- Desai AN, Majumder MS. What Is Herd Immunity? JAMA. 2020;324(20):2113. doi: 10.1001/jama.2020.20895
- W.A. Orenstein, & R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).
References
- Measles. World Health Organization. November 14, 2024. Link
- Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017 Dec;17(12):e420-e428. doi: 10.1016/S1473-3099(17)30307-9. Epub 2017 Jul 27. PMID: 28757186.
- Ridenhour, B., et al. (2018 Dec). “Unraveling R0: Considerations for Public Health Applications.” American Journal of Public Health 108(Suppl 6).
- R, T., et al. (2022 Sep). “Global variation in early epidemic growth rates and reproduction number of seasonal influenza.” International journal of infectious diseases: IJID122.
- Leung, N. H. L. (2021 Mar 22). “Transmissibility and transmission of respiratory viruses.” Nature Reviews. Microbiology 19(8).
- Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 7 Measles. CDC. May 13, 2019. Link
- Measles Vaccination: Know the Facts. Infectious Disease Society of America. November 25, 2024. Link
- Measles Symptoms and Complications. CDC. May 9, 2024. Link
- Measles vaccination coverage. World Health Organization. Link
- Desai AN, Majumder MS. What Is Herd Immunity? JAMA. 2020;324(20):2113. doi: 10.1001/jama.2020.20895
- W.A. Orenstein, & R. Ahmed, Simply put: Vaccination saves lives, Proc. Natl. Acad. Sci. U.S.A. 114 (16) 4031-4033, https://doi.org/10.1073/pnas.1704507114 (2017).